What is menopause?
Menopause is when the ovaries stop releasing eggs and menstruation ends for good. A woman has officially entered menopause on the 365th day from the date of her last menstrual period.
However, women’s transition to menopause is usually gradual and involves fluctuating hormone levels and a range of symptoms for several years.
Female hormone “operation shut down” actually begins during the late twenties, but isn’t really evident until between the ages of 35 to 45 years. This is when many women start to notice changes in their bodies, minds, and feelings. Periods become irregular, the libido tanks, and counting sheep no longer helps with sleep. And hey, did someone turn up the thermostat?
A shared yet diverse experience
One study, for instance, found that even in the same region, women’s symptoms varied by ethnicity.
American women of European descent reported more psychosomatic symptoms (e.g. moodiness, irritability, forgetfulness), while women of Asian descent reported more vasomotor symptoms (e.g. heart palpitations, hot flashes, etc.). Women of Asian descent reported much lower symptoms overall. Researchers also found that symptoms varied depending on the stage of menopause.
Thus, the researchers argued, there is probably no such thing as a universal “menopause syndrome”.
While there are common symptoms that many women experience (see below), and an official definition (see above), it’s important to understand that each woman’s experience of menopause is unique.
Symptoms of menopause, perceptions of menopause, and age of onset vary widely from woman to woman, region to region and by ethnicity. This is probably due to differences in
- lifestyle
- diet
- genetic factors
- reproductive history and pregnancy (for instance, on average African women have more children and hit menopause earlier than their counterparts of African descent living in the U.S., which researchers think may be due to demographic patterns of earlier and more frequent pregnancies)
- cultural factors: each culture and social group views menopause differently, which affects how women think about their own symptoms and experiences
- social factors: women have other life challenges, changes, and demands during midlife
In the U.S., about 85% of women will have entered menopause by age 52. With the population of older folks increasing in developed countries, more women are menopausal and post-menopausal.
When is too soon?
Since there’s no specific age of onset, and women’s experiences are diverse, it’s hard to define exactly what “premature” menopause is. However, if women have low sex hormone levels and their periods check out before age 40, that’s officially considered “premature”.
We don’t yet know why premature menopause occurs; it could have an autoimmune component and has been linked to other autoimmune disorders such as thyroiditis and fibromyalgia. Chances of premature menopause also go up with smoking, ovary damage (e.g. from surgery), genetic predisposition, and exposure to xenoestrogens.
What you should know about menopause
Ovaries produce estrogen, progesterone and androgens. They are signaled to do so by FSH (follicle stimulating hormone) and LH (luteinizing hormone) from the brain. With menopause, these hormones gradually decrease.
With advancing age, muscle mass and bone mass can decrease, which can influence other hormones in the body, leading to a decrease in GH, IGF-1, and DHEA.
As hormone levels change, so does the body. A perimenopausal woman should be on the lookout for:
- Loss of the menstrual cycle
- Hot flashes and night sweats
- Cardiovascular disease
- Osteoporosis
- Emotional changes
- Vaginal dryness/infections
- Incontinence/urinary tract infections
- Decline in sex drive
- Insomnia
Hormone production
As ovarian hormone production declines, sex hormones secreted by body fat and other organs such as the adrenal glands become more prevalent. The balance tips.
It’s important to keep your body fat in a healthy range with good nutrition and regular activity as you age. Having a lot of excess body fat puts your hormone production out of whack and creates systemic inflammation. That just makes things worse.
See All About Estrogens for more.
Hormone replacement therapy: A controversial option
Hormone replacement therapy (HRT) can offset low hormone levels in the body. Large studies have been completed that provide useful information about perimenopausal HRT, including the HERS study, the ERA study, and the Women’s Health Initiative Clinical Trial.
The Women’s Health Initiative Clinical Trial indicated that for women who are within 10 years of menopause who have taken HRT for 5 or more years, there is a 30% reduction in all cause mortality.
There are natural and synthetic options for HRT.
Natural hormones are substances identical to those produced in the body. Synthetic hormones are chemically altered so that companies can patent them, but still similar enough to the natural kind so they enter the cell and perform most of the same functions.
Only natural progesterone seems to help prevent cancers, normalize blood fats, restore sex drive and regulate sleep. Synthetic progestins can contribute to mood swings, fatigue, insomnia, bloating, weight gain, and anxiety.
Most published data on HRT relates to synthetic hormones, and many women’s health advocates have pointed out significant problems with using synthetic hormones, which are typically derived from non-human sources such as pregnant mares and not identical to the hormones already present in women’s bodies.
Based on available data, here’s how HRT — again, mostly with synthetic hormones — stands.
| HRT benefits | HRT risks |
|---|---|
|
|
The American Association of Clinical Endocrinologists announced in 2008 that the benefits of HRT in women under 60 years of age outweigh the risks, and the use of HRT is supported by the ACOG and North American Menopause Society.
Note: Many of the negative HRT effects seem to occur when using combination therapy (synthetic estrogen + synthetic progestin) vs. estrogen only.
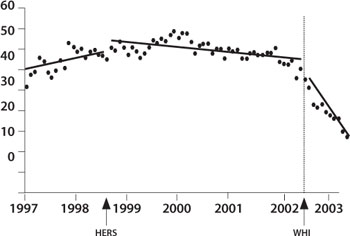
The image below shows HRT use among postmenopausal women between 1997 and 2003.
The first vertical line represents the publication date of the HERS study in August 1998 – you’ll notice a slight decrease in HRT use. The second vertical line represents the publication date of the WHI Clinical Trial in July 2002 – you’ll notice a sharp decrease in HRT use.
Why menopause is important
Most of the factors that accompany menopause are temporary, but some can be very harmful. Let’s highlight the biggies.
- Hot flashes/night sweats
- Cardiovascular disease
- Osteoporosis; decreased bone density
- Emotional changes
- Insomnia
“Power surge”: Hot flashes
Hot flashes aren’t really “harmful,” assuming they don’t harm your social life or light the bedsheets on fire. But they sure are a drag.
Some women never have hot flashes at all, probably because they are good at making estrogen from other sources like body fat and androgens.
Hot flashes usually last a few — seemingly interminable — minutes. During this time, skin temperature can actually increase by up to 8 degrees F. Core body temperature stays the same or decreases. Many women find that hot flashes are particularly bad at night.
Hot flashes often increase before menopause, peak 2-3 years after onset, and then taper off. Triggers include stress, coffee, spicy foods, alcohol, sugar, citrus fruits, high BMI, smoking, SSRIs, large meals, and intense exercise.
During a normal menstrual cycle, LH triggers the release of the egg from its follicle. But with decreased estrogen, the ovaries don’t respond.
Thus, the hypothalamus releases GNRH in order to stimulate the pituitary to send LH to the ovaries.
LH keeps signaling the ovaries with no response.
The body hits the hypothalamus with adrenaline since estrogen levels are low.
With all of this over-direction, the hypothalamus gets confused, resetting the body’s thermostat to reach a higher temperature.
Vessels dilate in the periphery and blood travels to the skin allowing the body to cool by evaporation and bringing the temp down.
Changes in serotonin and norepinephrine are associated with circulating estrogens and may contribute to hot flashes as well.
Soy and hot flashes
Just 25% of Japanese women experience hot flashes vs. 85% of North American women (although some researchers propose that these numbers might be skewed due to reporting bias).
Although there are probably many factors involved, such as genetics and other dietary factors such as fish/seafood consumption (which creates a higher level of omega-3 fatty acids), some think this variation is due to the consumption of soy.
Soy (and many other plant foods) contains isoflavones, a type of phytoestrogen, which are plant derived compounds that can exhibit hormonal activity. American women consume less than 3 mg of isoflavones per day, while women in Eastern Asia consume between 20 and 80 mg/day.
Consuming 50-100 mg/day of isoflavones from food seems to be a safe amount that helps to relieve hot flashes. This would be equivalent to consuming one of the following:
- 1 to 1½ cups soy milk
- 4-5 oz tempeh
- 4-5 oz tofu
- ½ cup edamame
- 3-4 tbsp miso
- ¼-1/2 cup soy nuts
However, flax meal may also be useful. One study showed that women suffering at least 14 hot flashes per week who added 4 tablespoons of flax meal per day to their diet for 6 weeks decreased daily hot flash frequency by 50%, and intensity dropped by 57%.
Some important notes:
Not all women efficiently convert phytoestrogens into a form the body can use to relieve menopausal symptoms.
Soy, like any food, can provoke hypersensitivity reactions. Some nutrition researchers note that soy can be allergenic or interfere with proper nutrient absorption and digestion.
If you are prone to thyroid and/or breast problems, as well as food intolerances, you might want to discuss eating more soy with a doc or dietitian first.
It’s best to get isoflavones from food rather than supplements. Isoflavone supplements might interfere with thyroid function and inhibit mineral absorption, so stick with whole food sources. Avoid consuming more than 150 mg of isoflavones per day.
Regular intake for 1-2 months is usually necessary to notice any effects from isoflavones.
Go with organic soy when possible.
The ACOG approves soy for relieving hot flashes.
Other options for hot flashes
Other options that might help to relieve hot flashes include:
- St. John’s wort (take caution as this herb interacts with various pharmaceuticals)
- yoga
- acupuncture
- massage
- meditation
- exercise
HRT is currently the only FDA approved treatment for hot flashes.
Options that don’t seem to help relieve hot flashes (and may cause additional problems) include:
- kava kava
- Dong quai
- evening primrose oil
- red clover
- ginseng
- black cohosh (Some cases of animal cancers have been reported, and there are 30 reports of serious liver damage with supplementation Mahady GB, et al. United States Pharmacopeia review of black cohosh case reports of hepatotoxicity. Menopause 2008;15(4 Pt. 1):628-638)
- wild yam cream (This contains progesterone precursors; yet humans lack the enzyme necessary to metabolize them. The only way to get true progesterone cream is with a prescription. OTC creams are fraudulent.)
Some menopause specialists simply recommend that rather than trying to eliminate hot flashes entirely, women integrate hot flashes into their daily lives: dress in layers, pop out for some fresh cool air if possible, etc.
Cardiovascular disease
Cardiovascular disease is the leading cause of death in postmenopausal women. Along with declining estradiol, as women age and put on body fat, they can develop insulin resistance/metabolic syndrome, which leads to Type 2 diabetes and further elevates their CVD risk.
While naturally occurring estradiol is cardioprotective, synthetic estrogen in HRT can lead to inflammation, blood clots, and be of no help to existing plaque on vessel walls.
To greatly decrease chances of developing heart disease as you enter menopause, do the following:
- Keep blood pressure below 120/80 mmHg
- Keep total cholesterol below 200 mg/dl
- Keep LDL below 70 mg/dl
- Keep HDL above 60 mg/dl
- Don’t smoke
- Manage stress and meditate
- Keep your body fat in a healthy range; don’t yo-yo diet
- Exercise at least 5 hours each week
- Consume plenty of whole, plant foods like vegetables, fruits, beans, whole grains, nuts and seeds
- Avoid processed foods and added sugar
- Include smaller amounts of alcohol, meat, fish, dairy, and eggs
- Drink tea and water
Osteoporosis
At menopause, calcium absorption is generally 50% below the adolescent peak rate. This is likely due to a lack of vitamin D (less time in sun, less consumed in diet, less uptake in gut).
Estrogen helps to slow bone breakdown and prevent factures by turning on vitamin D receptors in the gut (see more here: All About Vitamin D). HRT won’t help to build or replace bone, but it may help to prevent bone loss.
Ways to preserve bone mass upon menopause:
- Incorporate green leafy veggies, legumes and nuts/seeds – these seem to be the optimal sources of bone building calcium
- Get adequate sunlight to attain vitamin D (see more here: All About Vitamin D) — and hey, fresh air and exercise help relieve hot flashes too! Win-win!
- Avoid excessive alcohol, salt, carbonated drinks, and caffeine
- Check your calcium supplementation – it might contribute to the progression of cardiovascular disease. It’s best to only supplement when you can’t get enough calcium from food and vitamin D status is adequate. In addition, many women eating standard Western diets are actually deficient in magnesium and other trace minerals (such as phosphorus), not calcium.
- Eat soy – soy can increase intestinal calcium absorption and protect bone cells
- Do weight bearing exercise (resistance training, walking, etc.)
- Don’t smoke
- Include foods from the allium family – these can protect bones and inhibit cancer development
- Avoid refined sugars/grains – these don’t provide nutrients, can diminish bone health, increase inflammation, and result in mood swings and fatigue
Recent research suggests that osteoporosis is less a disease of “not enough calcium” and more about systemic inflammation and poor mineral absorption, particularly from a diet high in grains and dairy and low in veggies. (See All About Dietary Acids and Bases). There is evidence that estrogen may affect inflammatory cytokines (cell signaling molecules).
Emotional changes
Many women notice emotional highs and lows. This is a scientifically detached and polite way of saying that many women sometimes feel like they’re going nuts.
Emotional symptoms can include:
- crying spells; sadness
- irritability and anger
- panic and anxiety; sense of dread or impending doom
- depression and lethargy
To ensure a stable mood:
- Incorporate plenty of whole foods rich in vitamin C like bell peppers, citrus fruits, broccoli, teas, potatoes, and yams
- Eat foods with B vitamins for the nervous system like wild rice, brown rice, quinoa, buckwheat, polenta, and green leafy vegetables
- Get outdoors for recreation
- Eat whole grains to bump up serotonin
- Eat regular meals
- Limit processed foods, added sugars, alcohol and caffeine
- Incorporate omega-3 fats from algae, flax, hemp, chia, and walnuts
- Address underlying factors, e.g. stress, relationship difficulties, etc.
Many women find that counselling is helpful during this period. Midlife is also a period of life change, and mood changes can reflect “real” changes, shifts in priorities or life demands, and/or underlying issues (such as changes in family dynamics or caregiving).
Recognize that these symptoms are common, and (in part) related to hormonal changes — you’re not going crazy!
Insomnia
This is often due to night sweats and/or anxiety, but generalized hormone fluctuations can cause sleep disturbances too. Along with changes in sex hormones, women may notice changes in other hormones such as thyroid and/or adrenal hormones.
To promote restful sleep:
- Limit alcohol (see here for more on this: All About Alcohol) – remember that alcohol can compromise liver function, diminishing its ability to metabolize estrogens
- Limit caffeine
- Try a small serving of starchy carbohydrates in the evening, which can increase serotonin
- Avoid protein, sugar, fat, beans, and liquids before sleeping
- Melatonin or valerian might help with sleep, but side effects can occur
- Basic sleep hygiene is in order; see All About Sleep for more
- Other hormonal conditions can affect sleep, so discuss any symptoms with your doctor or endocrinologist
There are social factors too. Many midlife women are struggling with competing responsibilities: paid work, unpaid work (e.g. domestic work), caregiving for children and aging parents, etc. It’s no wonder that many of them can’t sleep!
Other physical and mental changes
Hey, where did that spare tire come from? Why are you feeling more like an apple than a pear these days? Why doesn’t food X agree with you any more? Why is it so hard to lose fat? Why are you suddenly attracted to elastic waistbands? And where did you leave your freaking car keys??!
There are many other physical and mental changes that can occur in midlife, which again reflect changes in both the physical environment (i.e. hormonal changes) and changes in your personal life (e.g. caregiving stress). This includes:
- changes in sex drive
- vaginal dryness; yeast infections; bladder infections and interstitial cystitis
- changes in breast size (as estrogen declines) and comfort (e.g. tenderness, lumpiness)
- forgetfulness; “brain fog”; difficulty concentrating
- digestive changes; new food intolerances
- water retention; bloating
- increased intensity of PMS symptoms
- difficulty losing fat
- changes in appetite and/or food cravings
- dizziness; lightheadedness
- heart palpitations
- “inner tremor” or jitteriness; some women talk about it feeling like an “inside earthquake”
- headaches; migraines
- joint pain
- tingling, “electric shock” type pain in extremities
- fatigue; lethargy
- hair loss; thinning hair
- brittle nails
Summary and recommendations
Physical, intellectual, and emotional changes in midlife are normal for men and women. Changes take a variety of forms.
Each woman’s experience of menopause is unique. You can significantly affect your menopause symptoms with good nutrition and regular activity.
Symptoms are complex and inter-related. For instance, changes in digestion or the hormonal environment can affect fat loss. Insomnia can add to your stress, worsen your mood, and make you want to reach for that caffeine.
Build a strong support network that includes health care providers, coaches, counsellors, other women, family and friends, etc. Ask for help. Don’t go it alone.
Do your homework and learn about your experiences, as well as those of other women. Chances are, you’re not “abnormal”.
If menopausal symptoms are manageable, exploring natural options is likely the best option. For those with significant and debilitating menopausal symptoms, and under the age of 60, HRT might be something to consider.
Living, exercising, and eating the PN-style way can help control symptoms and decrease chances of potential diseases associated with menopause. This includes:
- Keep your body fat in a healthy range; don’t yo-yo diet
- Exercise at least 5 hours each week, and include weight-bearing activities as well as stress-relieving activities such as outdoor walking
- Consume plenty of whole, plant foods like vegetables, fruits, beans, whole grains, nuts and seeds
- Include controlled amounts of alcohol, caffeine, meat, fish, dairy, and eggs
- Avoid processed foods, added salt, smoking, and added sugar
- Drink tea and water
- Consider eating small amounts of whole soy foods each day
- Manage stress and meditate
Extra credit
A hysterectomy will cause menstrual periods to stop, but it won’t induce menopause, because the ovaries continue to function.
Bloating with menopause/post-menopause can be due to changes in digestive abilities. Stomach acid tends to decrease. This can be alleviated with a digestive enzyme supplement, digestion tea with peppermint/ginger, limiting animal foods, using a probiotic rich food or supplement, and lightly cooking raw vegetables.
Taking a contraceptive pharmaceutical can mask perimenopuase by controlling typical symptoms. This doesn’t “change” the time of menopause for you.
Estradiol tends to suppress appetite.
The Japanese have no word for “hot flash.”
A plant-based diet is associated with fewer hot flashes.
Changes in estrogen might influence fat cell activity in the abdomen.
Men can experience hot flashes when testosterone suddenly drops, such as in prostate cancer treatment.
Current data provides assurance that isoflavone exposure at levels consistent with historical Asian soy intake doesn’t seem to result in adverse effects on breast tissue.
Cruciferous vegetables may guard against estrogen dependent cancers.
Seaweed has minerals for thyroid function and can inhibit cancer development.
References
Click here to view the information sources referenced in this article.
Learn more
Want to get in the best shape of your life, and stay that way for good? Check out the following 5-day body transformation courses.
The best part? They're totally free.
To check out the free courses, just click one of the links below.
Share