What is Vitamin D? | How Much Do You Need? | Vitamin D and The Sun | Food Sources | Best Supplement | Deficiency | Nutrient Interactions | Vitamin D and Immunity
Vitamin D is starting to sound, well, too good to be true.
Hundreds of research studies suggest that vitamin D can help prevent everything from osteoporosis to autoimmune disorders, cardiovascular disease, and cancer.1
Doctors are recommending it. Health podcasters are talking about it. Even your mom is nagging you about it.
Want all the key vitamin D facts in one easily-sharable resource?
Download our vitamin D "cheat sheet", which includes:
- A reference table that tells you how much vitamin D you need, depending on your stage of life
- A list of the best food sources of vitamin D
- A quiz to assess whether you're at risk of a vitamin D deficiency
If you’re a coach, this is a great handout or reference sheet for clients. And if you’re curious about vitamin D yourself, you’ll have the info you need at the ready.
With all the hype, many people are wondering:
“Should I take vitamin D?”
We have your answers.
In this article, we’ll show you how to figure out if vitamin D supplementation is right for you.
You’ll learn why it’s important for your health, how much you need, and what to know before you think about taking a vitamin D supplement.
(For coaches and practitioners: Check out our handy vitamin D “cheat sheet.” You can use it as a reference for yourself, or as a handout for clients.)
Oh, and when you’re done reading, you can send this article to Mom. (And give her our best, will you?)
What is vitamin D?
Vitamin D is a fat-soluble vitamin that we (mostly) get from the sun, but also from certain foods, and of course, from supplements.
And actually, “vitamin D” isn’t just one single thing. Vitamin D refers to a group of compounds.
Let’s meet the family:
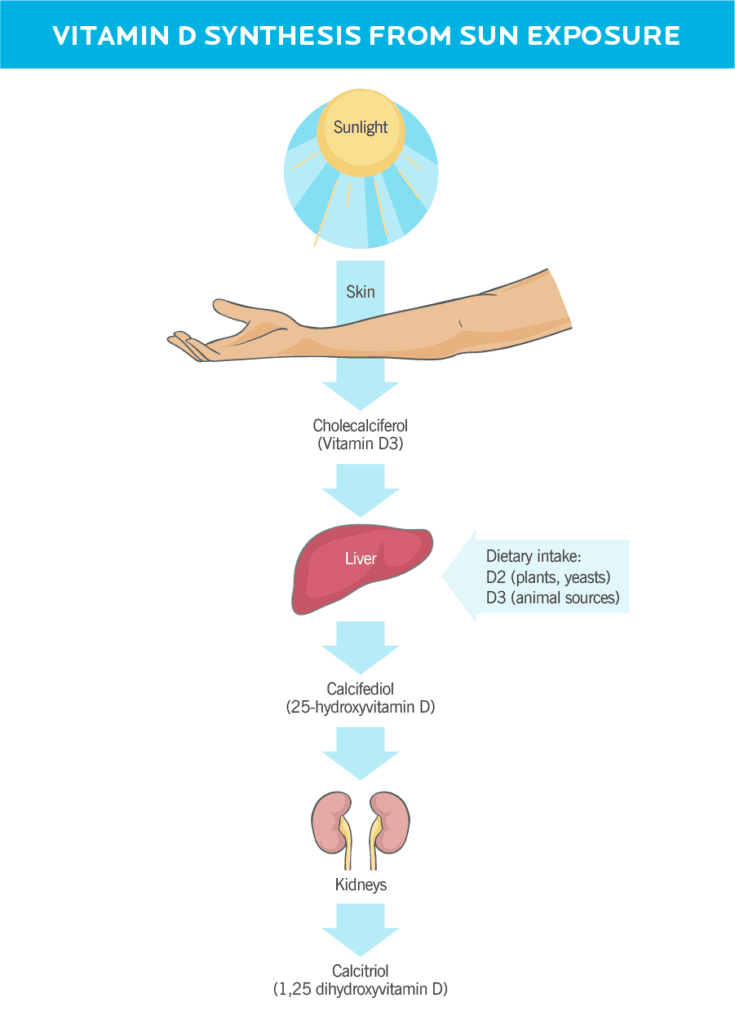
- Vitamin D2 (ergocalciferol) can be made by plants (such as mushrooms) and yeasts.
- Vitamin D3 (cholecalciferol) comes from animal products like fish, egg yolks, and cheese. We also make vitamin D3 on the surface of our skin when we’re exposed to sunlight.
- Calcifediol (25-hydroxyvitamin D) is the form of vitamin D that’s measured in blood tests. It actually starts out as vitamin D3, but once vitamin D3 enters your bloodstream your liver converts it into calcifediol.
- Calcitriol (1,25 dihydroxyvitamin D) is the most metabolically active form of vitamin D. It’s created in your kidneys from calcifediol. Unlike its precursor vitamin D3, calcitriol is no longer considered a vitamin: It’s a hormone.
Whoa. So much shape-shifting. Sneaky.
What does vitamin D do?
Recent research suggests that nearly every cell of our body has receptors for vitamin D. Not surprisingly, it has wide-ranging effects in the body.
Vitamin D helps support your:
- immune system
- cell function
- blood sugar regulation
- bone health
- calcium absorption and circulation
- normal blood pressure
(Did you know that most vitamins and minerals have broad health effects? Learn more: All about vitamins and minerals.)
How do I know if I need to supplement?
For many of us, supplementing with vitamin D is a good idea. Especially if we fall into one of the categories of people who are more likely to have a vitamin D deficiency. (Take the quiz below to find out if that’s you.)
However, the only way to know for sure if we’re deficient is to get a blood test.
In order to optimize bone health and minimize the risk of disease, people should aim to achieve a blood level of vitamin D of at least 50 nmol/L (20 ng/mL).2 (The “sweet spot” might be closer to around 75 nmol/L, or 30 ng/mL.)
To meet this target, here are the suggested daily vitamin D intakes (from combined food and supplement sources), for different stages of life:
General recommendations for vitamin D intake
| Age | Recommended daily vitamin D intake |
|---|---|
| 0–12 months | 400–1000 IU/d |
| 1–18 years | 600–1000 IU/d |
| 18–70+ years | 800–2000 IU/d |
| Pregnant / breastfeeding (>18 years) | 800–2000 IU/d |
Most healthy adults should be able to maintain an adequate blood level of vitamin D (50–100 nmol/L or 20-40 ng/mL) by getting about 800-1000 IU daily of vitamin D, from both food and supplement sources.
In cases of more severe deficiency, some people may need to take more vitamin D than we’ve listed above. Work with your medical doctor to figure out the right dose for you, and how long to take it for.
How do you get vitamin D?
The best vitamin D source, ever: The sun
Many people can meet their vitamin D requirements through sunshine alone. And as far as “natural sources of vitamin D” goes, sunlight is a tippy top choice.
A good general guideline: Get about 10-20 minutes a day of midday sun, with face, arms, hands, and legs uncovered (and no sunscreen).
The amount of vitamin D you get (and absorb) from the sun depends on a bunch of things, like geographic location, skin tone, clothing style, sunscreen use, age, and overall health.
So, depending on who you are, and where you are, you may need more sun than the above recommendation.
The best vitamin D food sources
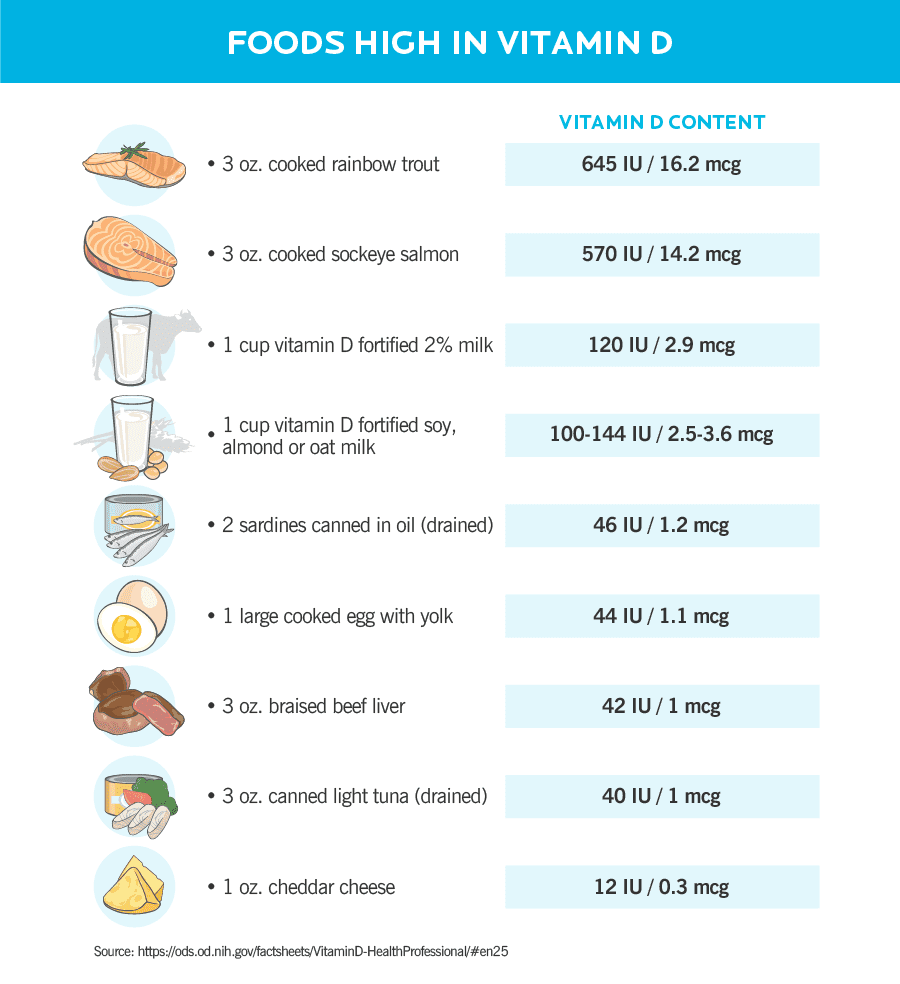
You can significantly bump up your vitamin D intake by prioritizing certain foods in your diet.
Here are some of the best sources3:
The best vitamin D supplement
Vitamin D supplements can come as a pill, liquid, sublingual spray, or (yes) chewable gummy worm.
While the delivery method of the supplement isn’t so important4, the form of the vitamin D in it is.
Usually, you’ll find two forms of vitamin D available in pharmacies and health food stores:
- Vitamin D2, derived from yeast or mushrooms (and vegan-friendly)
- Vitamin D3, typically sourced from lanolin (from sheep’s wool)
While both forms can raise blood levels of vitamin D, vitamin D3 appears to do a better job of optimizing vitamin D levels, as well as maintaining these levels longer-term.5,6,7
So, unless you’re avoiding animal products, look for a supplement that contains vitamin D3 (cholecalciferol).
However—and this is important—taking vitamin D when you’re not deficient will have little to no benefit—and may even cause harm.8
(More on how to assess your risk of deficiency below.)
The interaction between vitamin D, calcium, and other nutrients
Meet vitamin D’s “colleagues.”
The following nutrients support vitamin D’s role in the body, as well as mutually benefit from vitamin D’s presence.
- Calcium is absorbed better in the presence of vitamin D. That’s one of the reasons vitamin D is important for bone health. But, taking too much of both can cause calcium to build up in places where it doesn’t belong: soft tissues like the kidneys and arteries.9
- Vitamin K helps direct calcium to where it’s supposed to go (mostly, the bones).10 Taking vitamin K with vitamin D may prevent calcium from depositing into the soft tissues.11,12,13
- Magnesium may help convert vitamin D to its more metabolically active forms. Research shows that taking magnesium with vitamin D is more effective at correcting a vitamin D deficiency than vitamin D supplementation alone.14,15
- Vitamin A can prevent vitamin D toxicity, and vice versa.3 Also, some studies suggest that increasing vitamin A can reduce the calcium buildup that can happen with higher levels of vitamin D.16
There’s one caveat here: Taking high doses of vitamin D along with high doses of any of these vitamins and minerals can, in some cases, backfire and contribute to health problems. (Especially if you have other nutrient deficiencies.)
While it’s very unlikely to “overdose” on nutrition from food, supplements can allow you to mega-dose, and that’s where potential issues could arise.
If you’re unsure about how to balance your supplements, talk to your medical doctor.
Vitamin D deficiency
Most experts agree that having a blood level of:
- 30-50 nmol/L (12-20 ng/mL) of 25-hydroxyvitamin D3, or 25(OH)D is insufficient for optimal health
- <30 nmol/L (12 ng/mL) of 25(OH)D is considered a severe deficiency
Levels in both of these ranges likely benefit from supplementation.17,18,19
How common is vitamin D deficiency?
Statistics suggest that between 20 and 40 percent of adults and children worldwide have insufficient levels of vitamin D.19,20,21
Now here’s a fun quiz (well, fun for health nerds like us):
If you answer “yes” to any of the following questions, you’re at an increased risk of vitamin deficiency.
Do you:
- Live far from the equator, and/or experience winter? It’s nearly impossible to get enough vitamin D from sunlight during certain seasons—usually the colder months—even if you spend lots of time outside.22
- Have darker skin? Melanin—the pigment that makes skin dark—reduces the skin’s ability to produce vitamin D when it’s been exposed to sunlight.17 In the US, 89 percent of Blacks and 69 percent of Hispanics are deficient in vitamin D.23
- Fall into the “50+” age category? Age decreases the body’s ability to synthesize vitamin D on the skin.24
- Have a chronic illness, malabsorption issues, or have a BMI that categorizes you as “obese”? People with certain illnesses, malabsorption, or obesity don’t necessarily have trouble making vitamin D on the skin, but they’re more likely to have issues absorbing and metabolizing it.25,26
- Tend to cover up when you go outside (either with clothing or sunscreen)? Wearing clothing that covers most of your body—for religious, style, or health reasons—or wearing sunscreen, protects your skin from UVB and UVA light, blocking vitamin D synthesis. Burn or skin cancer survivors may be especially prone to slathering up with SPF.
- Just not go outside much (during daylight)? Whether due to illness or shift work, if you’re not able to go outside when the sun is highest, you’ll miss the window for optimal vitamin D synthesis.
Diseases associated with vitamin D deficiency
As you might imagine, the worse a deficiency is, the more likely negative health effects start to show up.
More extreme deficiencies of vitamin D dramatically increase the risk of premature death, infections, and many other diseases.27
Some diseases associated with vitamin D deficiency:
- Osteoporosis, and general weakening or softening of the bones26
- Immune dysfunction, such as autoimmune conditions and increased susceptibility to infection28
- Type 2 diabetes29,30
- Cardiovascular disease31,32
- Cancer, especially cancer mortality33,34,35
- Obesity36
- Depression37
Problem is, we don’t have clear evidence that improving vitamin D status alone reverses or improves these conditions. Nor do we know for sure if vitamin D deficiency or insufficiency is actually what causes them in the first place.
Although vitamin D deficiency is related to these conditions, we’re still trying to figure out how.
Vitamin D and Immunity
For years, vitamin D has been touted as an immune booster.
As a result, it’s become a popular “just in case” supplement during flu seasons, and even more so during the COVID-19 pandemic.
But remember how we said that supplementing with vitamin D won’t likely benefit you if you aren’t deficient?
That applies to immune function too.
Taking extra vitamin D when your levels are normal won’t give you “super immunity.”
Yes, some research shows vitamin D deficiency is linked to more frequent and more severe infections—like upper respiratory tract illnesses38 and COVID-19.39,40
So if you’re worried about your immune health and you suspect you have a vitamin D deficiency, get tested.
If you have a confirmed deficiency, get those D levels into a normal range: 50-100 nmol/L (20-40 ng/mL) of 25(OH)D.
(Your doctor can help you figure out the right dose of vitamin D, and how long to take it for.)
On the other hand, if your vitamin D levels are normal, the current scientific evidence suggests there’s no reason to supplement.
Learn more: 8 ways to optimize your immunity and protect your health.
Vitamin D: Your next steps
1. If possible, get some (safe) sun exposure, and aim to eat vitamin D-rich foods.
Many people’s vitamin D requirements can and should be met through sun exposure and diet alone.
Eat vitamin D-rich foods, along with a range of colorful fruits and veggies high in vitamins and minerals—like calcium, magnesium, vitamin K, and vitamin A—that support vitamin D’s work in the body.
As a coach, unless you have another designation that qualifies you to practice Medical Nutrition Therapy (MNT), you’re best to stick with food and lifestyle practices to help your clients meet their vitamin D requirements.
Coaches can educate clients about their risk factors, or provide general guidelines for vitamin D intake, but only qualified MNT practitioners can diagnose and treat deficiencies.
2. If you suspect a deficiency, get a blood test.
When possible, get a blood test to confirm suspected deficiencies. (That goes for other nutrients too—like iron or vitamin B12—not just vitamin D.)
And, remember that in the presence of other deficiencies, we should be careful about supplementing with high doses of vitamin D.
Consult a doctor to help you determine if there’s a deficiency, and if so, what dose to take to remedy it.
3. Be mindful of those who are more vulnerable to deficiency.
If you have a client who:
- has malabsorption issues
- has darker skin
- lives far from the equator
- covers up (either with clothes or sunscreen)
…know that vitamin D deficiency is common.20
And most people low in vitamin D won’t “feel” it.
While some might get colds or flus a bit more often,42 many people don’t have any symptoms at all.
If a client falls into one or more of the “at risk” categories (especially if their diet is also low in vitamin D food sources), it’s not a bad idea to suggest that they work with a doctor, and get tested.
The bottom line: Even if something is essential to our health—like vitamins, minerals, water, and, oh, let’s say, a good stash of toilet paper—more isn’t always better.
References
Click here to view the information sources referenced in this article.
If you’re a coach, or you want to be…
You can help people build sustainable nutrition and lifestyle habits that will significantly improve their physical and mental health—while you make a great living doing what you love. We'll show you how.
If you’d like to learn more, consider the PN Level 1 Nutrition Coaching Certification. (You can enroll now at a big discount.)




Share