Good health and a killer bod might come naturally in your 20s… but what about your 30s, 40s, 50s, 60s, and yes, even 70s? Here’s how to eat right for your age and feel great at every stage of life.
- Want to listen instead of read? Download the audio recording here…
++
Growing up ain’t easy.
Whether you’re just entering ‘the real world’ after college, doing the kids-and-career-dance, or preparing for retirement, all stages of life have their surprises and curveballs.
In the words of Ferris Bueller, “life moves by pretty fast.” Nothing stays the same for long. And sometimes it can feel hard to keep up.
This goes for health and fitness, too.
As we age, our bodies change. (Yes, 20-somethings, this will actually happen to you.) Our focus changes. Our motivation changes. Our nutritional needs change. Our activity habits and abilities change.
How do we adapt? And keep up the awesome even as we age?
How do we make the best of where we are, right here and now?
The trick is to focus on the right things at the right times. By giving our bodies what they need today, we can help ourselves stay as healthy and vibrant as possible.
Here’s a quick guide to your best healthy habits to make the most of each life stage. But first a quick note…
Age categories are less meaningful or fixed than they used to be. Your age might not align with the commonly presumed life stage.
For instance, you may come into parenthood unusually early or late in life.
Or you might be an advanced senior with no immediate plans for retirement.
Or you may have habits that are accelerating your biological aging or slowing it down.
Wherever you’re at, there are some pretty universal standards that apply. We call these foundational health habits. These are useful for everyone.
Then there’s the special age-related stuff.
Different decades bring unique features. Sometimes these “unique features” are interesting, or even rewarding. And sometimes they really suck.
That’s where fine-tuning your exercise, nutrition, and other health habits can really help. This guide shows you how.
Feel free to read the whole thing from top to bottom. Or jump to the section most relevant to you by clicking one of the links below.
- The 20s: Building and exploring
- The 30s: Finding your groove
- The 40s: Still going strong
- The 50s: Refocusing and renewing
- The 60s: Second wind
- The 70s: Making a contribution
The 20s: Building and exploring

The good stuff:
In our 20s, our bodies are biologically at their peak in many ways. For example:
- We recover relatively quickly and well.
- Our bodies are pretty forgiving. We can get away with a lot of shenanigans, such as drinking a little too much, eating a little too much junk food, or skipping a few workouts.
- We can build bone, muscle, and connective tissue relatively easily and rapidly.
- We’re at our most fertile, hormonally speaking, and often looking for love.
We’re also exploring and trying stuff — new educational opportunities, new career opportunities, new relationship opportunities, new identities and life situations.
It can feel like anything is possible… and your body seems to agree.
The challenging stuff:
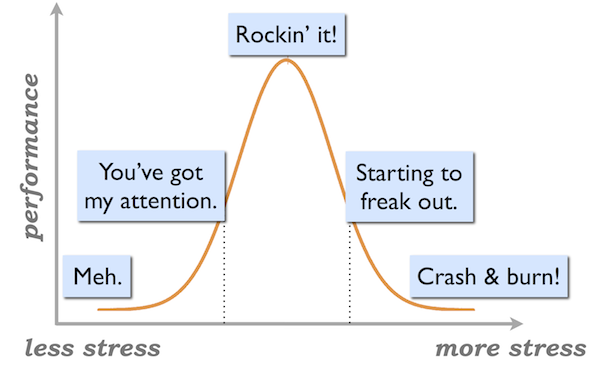
You might be combating the stress of trying to “make it” in school or the early stages of a career.
In particular, if you’re a competitive athlete, you can probably expect that most of your top performance will occur in your 20s; perhaps your athletic career might even be over by your early or mid-20s. That’s a lot of pressure.
Another common stressor at this age: looking good. The need to look a certain way might be a big motivator for you right now — and that can come with its own dose of stress and pressure.
Your best health habits right now:
In your 20s, some of the best things you can do for your health and fitness may include:
- Start to build your “owner’s manual.” Now that you’re out on your own, learn the fundamentals of exercise and nutrition choices and how they work for you. What is important to you? What are your goals? What healthy habits make sense for you and your life?
- Look for simple, general habits that you can still follow on a small budget or transient living arrangements (such as living in a student dorm).
- Weight train regularly and get enough protein. (Yes, this goes for both men and women!) Your 20s is a great time to build muscle, bone, and strong connective tissues: you’re building a foundation for your body that will last the rest of your life.
- Consider a variety of activities. Cross-training will build a solid foundation of movement, and it will help you explore a wide range of options to see what you enjoy the most. This is especially important if you’re an athlete, as it will provide a great base for future development.
These aren’t too complicated; the principles of healthy living never really are. However, implementation is always a challenge. For your next steps, click here. Or click here to learn more about coaching with us.
The 30s: Finding your groove

The good stuff:
In your 30s, you might find you’ve accumulated more self-knowledge… you may have a clearer sense what’s important to you in life — and a little more confidence to chase it.
You might be taking on some big, rewarding endeavors in your life: like career advancement, or raising children (or both).
Healthy habits might become a little more important to you now.
And you might have a little more stability and income. In other words, you probably have a bigger grocery budget and something nicer than a secondhand beer fridge to store it in.
The challenging stuff:
In our 30s, most of us are still feeling pretty good, but noticing some small physical differences. For example:
- Maybe it’s not quite as easy to lose body fat or gain muscle.
- Maybe things feel just a little achier or creakier in the morning.
- Maybe it takes you an extra day or two to recover from a tough workout.
Also, life might feel a little more ‘complicated’.
You might find you have more demands on you. More responsibility. And less time to work out and eat properly.
You may also have more mouths to feed, literally.
Your best health habits right now:
In your 30s, you may find that you need to:
- Adjust your caloric intake and activity levels to account for a slightly slower metabolism. (Remember how you used to be able to consume all that pizza and beer and never gain a pound? Those are now the good old days.)
- Be more careful with the quality of your intake. Your body might be a little more sensitive to what you feed it. For example, you may find you can’t tolerate alcohol as well.
- Optimize your hormonal (and overall) health if you are planning on starting or growing a family.
- Establish simple nutrition and fitness routines that juggle many demands (e.g. quick, effective workouts or fast-prep healthy dinners).
- Include de-stressing type activities as part of your exercise routine.
Sure, a little more to think about than your 20s. However, a little extra goes a long way at this stage. For your next steps, click here. Looking for some coaching and support? Learn more about PN Coaching.
The 40s: Going strong
The good stuff:
Your 40s are the start of early mid-life. Famous for being a bit of a roller-coaster, this decade can bring lots of satisfying experiences, which may include:
- Gaining confidence; more willingness to say ‘yes’ to what you really want and ‘no’ to the stuff you don’t.
- New, exciting levels of career development or professional success. Maybe even the guts to take some risks and try things you were afraid to do before.
- Deepening relationships with loved ones, possibly including children.
For some people this can be a time of personal growth. When it comes to health and fitness, that may mean improving healthy habits, devoting more time and energy to de-stressing, or fine-tuning some routines that will you allow you juggle all those balls in the air.
Meanwhile, you may feel great physically. (Especially if you’re active and taking care of yourself.) It’s still very possible to kick ass in your 40s!
The challenging stuff:
Chickens are coming home to roost. Your earlier choices are starting to show long-term effects.
You may really be noticing the effects of a slower metabolism, sarcopenia (age-related muscle loss) and changing body now.
You may notice things like:
- Minor aches and pains becoming more persistent.
- Small nagging health problems, or things taking longer to heal.
- Reduced levels of many hormones (such as thyroid or sex hormones).
- Having a harder time building strength / muscle, or losing fat; shifts in where you store your body fat.
- Declining athletic performance (even if you’re awesome, you probably won’t be competitive against 20-year-olds at the elite levels).
- New food sensitivities and intolerances.
If you’re female, you may be noticing some early ups and downs of perimenopause, the period before menopause when hormone levels decline and/or become a little more erratic. (For some women, this process can start in their 30s.)
If you’re male, you’re likely noticing lower testosterone.
Regardless of gender, you may have had one or more good old-fashioned mid-life crisis where you questioned your priorities along with your beliefs about yourself and the world. (On the upside, you have that shiny new sports car in the driveway.)
Your best health habits right now:
In your 40s, you may find that you need to:
- Keep adjusting your caloric intake as your metabolism continues to slow down.
- Spend more time on strength / resistance training to slow muscle loss as well as to maintain insulin sensitivity (which helps regulate blood sugar and prevent Type 2 diabetes).
- Spend more time on mobility, “pre-hab” types of activities, warming up, and active recovery.
- Consider your nutrition more carefully. That can mean focusing more on quality food choices and prevention of chronic disease, including:
- nutrient-rich foods such as colorful fruits and vegetables.
- a wide range of food types that cover the nutritional bases.
- Eliminate certain foods that now bother you, while adding others that help control inflammation (such as foods rich in omega-3 fatty acids).
- Supplement with a good probiotic as digestion starts to change.
- Practice mindful eating in the midst of life’s whirlwind.
Many of us here at Precision Nutrition are in our 40s. So we know this phase all too well. For more “fitness at 40” steps, click here. Or click here to learn more about coaching with us.
The 50s: Refocusing and renewing
The good stuff:
People in their 50s and 60s often report a renewed sense of purpose and vitality as they let go of earlier self-images and look ahead to the next phase of life.
They’re “over themselves” and don’t feel so pushed and pulled by many stressors that 20-somethings might struggle with, such as pleasing others.
This can be a time to find balance in your life, as well as focus on a larger purpose. The things that matter most to you start to come into focus.
Case-in-point: Many folks check out our PN Certification later in life when they feel like they have something to offer as mentors and guides, and when they want to work on their own terms.
The challenging stuff:
In your 50s, some physical signs of aging are definitely starting to pop up.
Joints are now creaking and crunching. Formerly lean parts may be a bit squishy, even if you’re fit. Your favorite foods now give you heartburn.
Your circadian rhythm may have shifted. While you might have partied to 5 AM in your 20s, you’re now finding 5 AM is your normal wake-up time in your 50s.
If you’re female, you’re likely noticing pre-menopause or menopause symptoms; if you’re male, you’re likely noticing lower testosterone.
Your work in the gym might have more to do with rehabbing injuries and controlling inflammation than showing off your killer abs.
And, um, by the way, when did the print on everything get so small?
Your best health habits:
To be at your best in your 50s, you may choose to incorporate some of the following habits:
- Keep adjusting your caloric intake as your metabolism continues to slow down.
- Make an effort to get essential fatty acids to keep your brain sharp and other fatty tissues such as eyes healthy. (Omega-3 fatty acids in particular help fight the inflammation underlying many chronic diseases.)
- Eat colorful fruits and vegetables; the carotenoids and other pigments help fight oxidative stress and reduce the risk of chronic diseases.
- Try evidence-based anti-inflammatory supplementation, such as:
- bromelain
- garlic
- turmeric
- cocoa, tea and berries.
- Watch your blood sugar levels and stay moving. Regular activity helps keep muscles strong as well as regulate glucose / insulin levels to prevent Type 2 diabetes.
- Keep on enjoying your favorite fitness activities, but factor in more time for mobility, “pre-hab” types of activities, warming up, and active recovery.
- Focus on nutrition, with an orientation towards quality food choices and prevention of chronic disease, such as:
- nutrient-rich foods such as colorful fruits and vegetables.
- a wide range of food types that cover the nutritional bases.
- Enjoy mindful eating as part of an overall “refocusing” and enjoyment of life.
More to think about than in your 40s, for sure. But, for many of us, it’s well worth the investment. Now’s the time to prepare for our health and abilities after retirement. For your next steps, click here. Looking for some coaching and support? Learn more about PN Coaching.
The 60s: Second wind

The good stuff:
While previous generations tended to slow down around this age, being in your 60s today is a lot different. (60 is the new 40, after all!)
Older people are more engaged than ever. In fact, your 60s can be a time to learn new things, have fun, and go on adventures.
You might be seeking new challenges, new opportunities, new ideas—but more meaningful ones. For many, this is a time of personal fulfillment.
Staying active during this time is a way to help maintain brain health, and overall physical function. But it’s also a gateway to personal fulfillment.
The challenging stuff:
It’s on now. You can’t argue with aging anymore.
Some days, it feels like you’re living in a different body—one you don’t recognize. It’s almost like a second puberty, where physiological stuff is just randomly happening without your prior knowledge or consent.
On the plus side, you’ve probably started to reconcile yourself to it, and are looking forward to the opportunities that experience and wisdom bring.
Your best health habits:
This is a great time to take on new challenges. You might have a bit more time on your hands now, so why not explore? Try some things? Challenge yourself?
Learning and novelty are important for brain function—and overall satisfaction.
Here are some other practices to consider:
- Focus on high-quality, nutrient-rich nutrition that helps you meet health challenges, such as:
- inflammation and pain (for instance, supplementing with Omega-3 fatty acids or removing foods that cause flare-ups).
- poorer digestion (for instance, adding sublingual vitamin B12, a digestive enzyme, probiotic, and/or fiber supplement).
- decreased or disrupted metabolism (for instance, adjusting how much you eat, or getting on a regular meal schedule).
- Exercise that helps you stay active, strong and vibrant while accommodating physical limitations or reduced recovery. For example:
- maintaining lean muscle mass and bone density with resistance training (plus activity with impact, if you can tolerate it; walking and running included.)
- balance, mobility and flexibility-promoting activities such as yoga or Tai Chi.
- rehabbing injuries or recovering from regular workouts with water-based exercise like swimming, water jogging, or Aquafit.
- activities that take some load off lower body joints while still giving you a good workout, such as cycling or rowing.
- trying new activities that are challenging, interesting and fun.
- Find some new healthy routines to help you cope with life transitions, which can include parents aging / dying, kids leaving home, job changes or retirement. You might join a local running group. Or get a dog — and walk it. Or travel somewhere new with a friend.
- Make sure you have your bases covered. Your annual check-up. Your regular dentist visit. Do your due diligence and check out those lumps and bumps.
Take advantage of this opportunity to do the things that bring value to your life. For a few next actions you can start today, click here. Or click here to learn more about coaching with us.
The 70s: Making a contribution

The good stuff:
People in their 70s are more likely than younger people to say they’re able to be present in the moment.
You might find you’re more conscious that health is a precious commodity and life is finite.
Simple pleasures in life — such as spending time with family and friends — may feel more enjoyable and rewarding.
This means lots of health, fitness, and nutrition opportunities. Many 70-somethings expect to stay just as active (perhaps differently so) as they did when they were younger.
Your 70s can also be a time to pass on wisdom, help others, or make financial contributions. For many, it is a time to reap the reward of hard work by seeing the positive influence they have made.
The challenging stuff:
If you’ve gotten this far without at least one major or minor health scare, you’re in a small minority. Many people find they’re taking a lot more supplements and drugs, and seeing a lot more doctors, than ever before.
As people age, they often become less active.
This sets up a vicious cycle where the normal effects of chronological aging are reinforced (and worsened) by inactivity: Physical function declines, dense muscle and bone disappear, falls become more common, and doing even everyday tasks can become more intimidating.
Digestive function decreases even more, along with oral health. Even small factors like declining smell, taste, and saliva production can affect food choices.
Your best health habits:
At this age, some important health habits may include:
- Compensating for decreased digestive function and absorption by:
- supplementing with digestive enzymes and possibly some types of sublingual vitamins
- increasing fiber intake to help gastric motility
- Packing more nutrition into smaller meals, since many folks in their 70s notice their appetite declining.
- Possibly adding a multi-vitamin / multi-mineral supplement, since nutrient deficiencies go up sharply in later life.
- Doing some exercise that includes “functional strength” and balance to stay strong in daily life and prevent falls; and weight-bearing exercises to maintain bone density.
- Doing some exercise that includes socializing and building relationships, such as a group exercise class or a hiking group.
- Incorporating social activities into daily life — which may include volunteer work or something that resonates with you. Community and connection become even more important as we age. The research is clear: once our relationships and sense of meaning decline, so does our health.
What to do next
As we’ve said, the above life stages are just a general guideline: everybody is a little bit different.
Think about where you’re at in life today. What can you do at this stage to help make the most of wherever you’re at—and make ‘future you’ a little healthier and happier?
Here are some general recommendations for staying fit, strong, lean and healthy at any age:
Stay moving.
Many “normal” parts of aging are due more to inactivity than the march of time. Get and stay active, however you can.
Choose nutrient-rich foods that add value to your body.
Lean protein, healthy fats, colorful fruits and vegetables, etc. all help prevent chronic disease and promote health.
Avoid things that take value away from your body.
This will change over time. In your 20s, a night of partying or a junk-food binge might be no big deal. In your 50s, it might wallop you. Notice how your body responds to your intake and behaviors, and adjust your decisions accordingly.
Recognize what you can control, and what you can’t.
You can’t control time. You can’t control random health problems. But you can control your behaviors. Making healthy choices won’t make you immortal or invincible, but it’ll give you a fighting chance at awesome aging.
Build and maintain connection and community.
Whether you’re playing on a team at 21, swapping tips with other sleep-deprived parents at 31, or caring for aging parents at 55, having meaningful relationships and a strong social support network is an essential part of health.
Get coaching.
Life is complex, and your experiences are unique. If you’re wondering about what might be best for you, or how you might tailor your own nutrition and exercise plan to your individual needs, seek out support. Life can be pretty confusing; we can all use a little guidance sometimes.
Want some help?
If you’d like some help staying consistent with your exercise and eating plan, we’d be happy to help. In fact, we’ll soon be taking new Precision Nutrition Coaching clients.
You see, we accept new clients every 6 months, and coaching spots typically sell out in hours. However, those motivated enough to put themselves on the presale list get to register 24 hours before everyone else. Plus, they receive a big discount at registration.
So put your name on the list below—because, as always, spots are first come, first served, and when they’re gone, they’re gone.



Share