What is insulin?
Insulin is a peptide hormone secreted by the pancreas in response to increases in blood sugar, usually following a meal.
However, you don’t have to eat a meal to secrete insulin. In fact, the pancreas always secretes a low level of insulin.
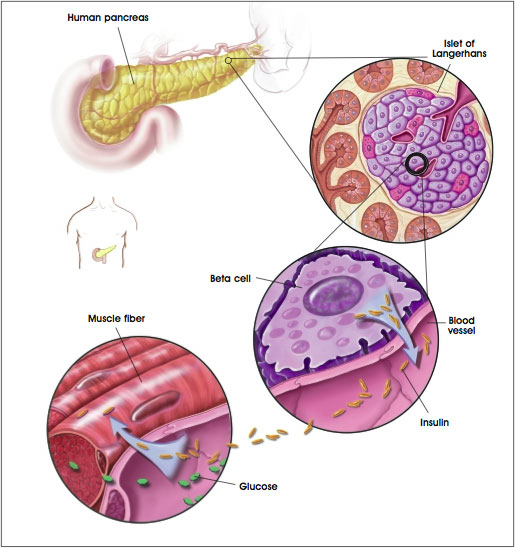
After a meal, the amount of insulin secreted into the blood increases as blood sugar rises. Similarly, as blood sugar falls, insulin secretion by the pancreas decreases.
Insulin thus acts as an “anabolic” or storage hormone. In fact, many have called insulin “the most anabolic hormone”. Once insulin is in the blood, it shuttles glucose (carbohydrates), amino acids, and blood fats into the cells of the body.
If these nutrients are shuttled primarily into muscle cells, then the muscles grow and body fat is managed. If these nutrients are shuttled primarily into fat cells, then muscle mass is unchanged and body fat is increased.
Insulin’s main actions
Rapid (seconds)
- Increases transport of glucose, amino acids (among the amino acids most strongly transported are valine, leucine, isoleucine, tyrosine and phenylalanine), and potassium into insulin-sensitive cells
Intermediate (minutes)
- Stimulates protein synthesis (insulin increases the formation of new proteins)
- Activates enzymes that store glycogen
- Inhibits protein degradation
Delayed (hours)
- Increases proteins and other enzymes for fat storage
Why is insulin so important?
The pancreas releases insulin whenever we consume food. In response to insulin, cells take in sugar from the bloodstream. This ultimately lowers high blood sugar levels back to a normal range.
Like all hormones, insulin has important functions, and an optimal level.
Without enough insulin, you lose all of the anabolic effects, since there is not enough insulin to transport or store energy or nutrients. Individuals with type 1 diabetes don’t produce insulin; if left untreated, they die.
On the other hand, if blood levels of insulin are always high, we also have trouble.
Continual elevation of insulin leads to large amounts of fat gain and risk for cardiovascular disease. This can lead to the development of type 2 diabetes.
Type 2 diabetes is characterized by obesity (particularly central deposition adiposity, or fat around the middle and deep in the abdominal cavity), cardiovascular disease, systemic inflammation, and the poor ability of muscles to store nutrients, which leads to muscle wasting and fat storage as well as nutrients circulating in the blood.
Insulin resistance, and its associated metabolic syndrome, is a step along the road to type 2 diabetes.
Like parents who may eventually tune out their screaming toddler, cells “tune out” insulin if insulin is chronically high. Since glucose is then poorly stored, people end up with both high circulating blood insulin and high circulating glucose.
Usually, they also end up with things like high triglycerides, high levels of “bad” LDL cholesterol, lower levels of “good” HDL cholesterol, higher levels of inflammatory proteins, and high blood pressure. Their blood is full of crud, their muscles aren’t getting properly nourished, and their body’s inflamed. It’s the perfect metabolic storm.

What you should know about insulin
Due to the anabolic power of insulin, many over-fat individuals want to avoid insulin release. This is because they want to avoid storing body fat. Well, as we already learned, you cannot avoid insulin in the blood.
You need insulin, but the trick is to learn how to balance the anabolic effects in muscle tissue against the fat storage effects. This can be done by increasing insulin sensitivity in the muscle while decreasing insulin sensitivity in the fat cells. Controlling insulin release during the day is important for long-term sensitivity.
What keeps insulin sensitivity high?
- Exercising 5 hours per week, especially resistance training
- Lots of muscle mass
- Higher intakes of vegetables, whole-grain foods, legumes, lean proteins, and nuts/seeds
- Supplements like omega-3 fatty acids, alpha-lipoic acid, and chromium
- Adequate vitamin D status
- Limiting caffeine intake
- Commuting to work via biking and/or walking
- Regular tea consumption
- 7-9 hours of sleep per night
What lowers insulin sensitivity?
- Low-carbohydrate, high-fat diets
- High processed carbohydrate diets
- Sedentary lifestyle
- Nicotine use
- Regular caffeine consumption
- Vitamin D deficiency
- Sporadic sleep patterns
- Excessive alcohol consumption
Summary and recommendations
- Participate in some form of resistance training and/or intense conditioning 4-5 times per week.
- Aim for a moderate carbohydrate consumption (~40% of diet) with an emphasis on fibrous carbohydrates like vegetables, fruits, legumes, and whole grains.
- Control fat intake (~20-25% of diet). Emphasize sources like nuts, seeds, olives, avocados, olive oil, flax oil, and fish oils.
- Investigate chromium and alpha lipoic acid, and make sure intake is adequate (but not excessive).
- Supplement with omega-3 fatty acids from algae or fish.
- Drink water or tea, and limit calorically dense beverages and alcohol.
- Make sure to get in the sun at least 20 minutes per day or use a vitamin D supplement.
- Make sure to get 7-9 hours of sleep per night.
For extra credit
Glycemic index and insulin index
While the glycemic and insulin indices of many foods are similar, some foods cause unexpected responses. Milk products have a lower glycemic index, but a very high insulin index. Rice has a higher glycemic index, but a lower insulin index. Keep in mind that a low glycemic diet can result in better fasted insulin and glucose, but results have been mixed.
Nutrient timing
The purpose of nutrient timing is to maximize insulin’s anabolic effects while minimizing its other problematic side effects.
Chromium
Chromium increases the presence of glucose transporters on the cell membrane. In theory, it may help manage blood sugar, but trials using chromium have shown mixed results.
Breast-feeding
Some epidemiologic studies have found that breast-feeding is associated with a reduced risk for developing insulin-dependent diabetes.
Early introduction of gluten-containing foods
Supplementing infant diets with gluten-containing foods before 3 months of age may encourage pancreatic dysfunction.
Nutrition and exercise patterns
Asian and African populations who are physically active and follow diets low in fat and high in fibrous carbohydrates have lower incidence of diabetes than those living the “Western” lifestyle.
Early introduction of cow’s milk
The American Academy of Pediatrics stated that avoiding early exposure to cow’s milk may reduce the risk of developing antibodies to cow’s milk protein and type 1 diabetes.
Alpha lipoic acid
Alpha lipoic acid may increase glucose uptake in the cell by recruiting glucose transporters.
Fat deposition patterns
Upper-body and central adiposity (in other words, fat around the middle and/or deep in the abdominal cavity) is strongly correlated with elevated insulin and, in excess, with metabolic syndrome.
Some people who are not obese by traditional measures are still at risk for insulin resistance anyway, particularly individuals with one or more close relatives who are diabetic, as well as many people of South Asian ethnic origin.
Insulin supplementation
Many bodybuilders have experimented with injecting insulin in an attempt to maximize insulin’s anabolic effects. This has sent more than one “home pharmacist” to the hospital, as even a little too much insulin in an injection can easily cause coma and death.
References
Click here to view the information sources referenced in this article.
Learn more
Want to get in the best shape of your life, and stay that way for good? Check out the following 5-day body transformation courses.
The best part? They're totally free.
To check out the free courses, just click one of the links below.

Share