The term probiotic comes from the Latin or Gree pro, “before, forward”, and bios, or “life” — thus probiotics are life-promoting.
In this case, we use the term probiotics to refer to beneficial bacteria.
We have billions of friendly bacteria living in our digestive tract. If you extracted all of the microbes that live in your body, you’d have over a quart of sludge. Each person’s bacterial flora may be as unique as fingerprints.
Friendly bacteria help us digest our food and absorb nutrients effectively. In a sense, we don’t actually digest many components of our food — the bacteria digest it.
The probiotic bacteria used in commercial productstoday are largely members of the genera Lactobacillus and Bifidobacterium.
Check out a food or supplement with probiotics and the label might say something like “Lactobacillus rhamnosus GG.”
The first name that appears is the genus (Lactobacillus).
The second name designates the species within the genus (rhamnosus).
The third name or number that appears is the specific strain within the species (GG).
Why are probiotics so important?
To understand why probiotics are important, we first need to understand how valuable beneficial bacteria are to our health, and how prevalent they are in our bodies.
What do gut bacteria do?
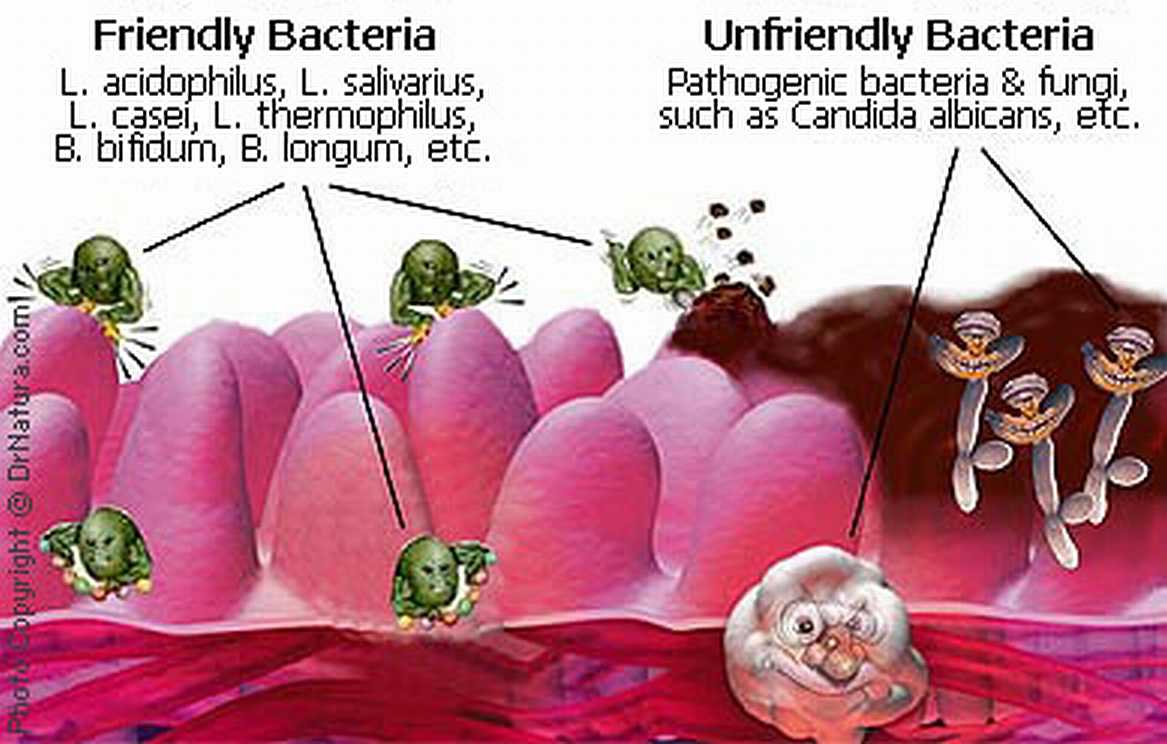
In our gut, good bacteria can displace bad bacteria and influence our overall health, metabolism, digestion, and body composition.
Gut bacteria are involved in immunity and help to ensure our immune system doesn’t have an itchy trigger finger (think food sensitivities).
Gut bacteria also:
- help synthesize B and K vitamins
- enhance gastrointestinal motility and function
- enhance digestion and nutrient absorption
- obstruct the growth of “bad bacteria” and other pathogens
- help metabolize other plant compounds/drugs
- produce short-chain fatty acids (SCFAs) and polyamines
- produce coagulation and growth factors
- produce cytokines (cell signaling molecules)
- help regulate intestinal mucus secretion and ultilization
- help regulate blood flow to the viscera
Uhmm… how much are in there anyway?
Imagine how many cells you must have making up your body. Zillions, right? Well, imagine 10 times that. That’s how many bacteria we have.
Our internal bacterial environment is very lively and complex. Scientists estimate that we have over 50 genera of bacteria that provide over 500 different species! There’s a party in our tummies!
Some researchers even suggest that our bacteria are like an entirely distinct organ — a “microbe organ” that is nearly as big and important (if not more so) than the liver.
Thus, given the extent of bacteria’s roles, and the importance of these good bacteria to proper physical functioning, it’s important for us to help keep a healthy bacterial environment.
Probiotics can help replenish and nourish this internal supply of good bacteria.
Adequate consumption of probiotics can help to eliminate abdominal pain, gas, bloating, reflux, allergies, nausea, food poisoning and vomiting. Probiotics may even alleviate irritable bowel syndrome (IBS), inflammatory bowel disease (IBD) and dermatitis. You guessed it – this means they are anti-inflammatory.
What you should know
What causes intestinal dysbiosis?
While our intestinal bacteria are pretty tough little critters, their health can be compromised. The most common causes of poor gut health are:
- medication use, especially antibiotics
- stress (stress hormones may encourage bad bacteria growth)
- poor diet (e.g. sugar, preservatives, alcohol, processed foods, over-eating, inadequate fibre)
- aggressive medical therapies such as radiation or chemotherapy
- over-consumption of animal-based protein, especially highly processed (e.g. luncheon meats)
- poor gut motility (which can be caused by the above factors)
One important feature of a healthy GI ecosystem is balance. When good bacteria flourish, bad bacteria and other micro-organisms such as yeasts and fungi are pushed out.
And speaking of diet, if you eat animal foods, the gut health of the animal is important too. When animals used for meat/dairy consume pre- and probiotics, they have healthier guts and bodies.
What makes probiotics?
Most often, probiotics are created via fermentation. Friendly bacteria are all around us — you’re soaking in them! — so fermentation simply collects them and gives them a nice place to grow. Fermentation organisms produce alcohol, lactic acid, and acetic acid, preservatives that retain nutrients and prevent spoilage.
Probiotics are found in yogurt, buttermilk, kefir, sauerkraut, kimchi, and bacterially cultured cheese. Traditional methods of meat preservation (such as the curing of salami) also use fermentation of Lactobacilli to preserve the food, although arguably industrially produced cured meats no longer have health benefits.
Benefits of fermentation
Fermentation not only bumps up good bacteria but helps eliminate anti-nutrients. When grains, seeds and tubers are soaked, sprouted and/or fermented, we disable anti-nutrients. This is good. It means:
- The food is more digestible (think tempeh instead of soybeans or yogurt instead of milk)
- The food has more minerals (thanks to less phytates)
- The food has more protein (thanks to less protease inhibitors)
And vitamin B12 is a product of bacterial fermentation. So, fermenting can create a reliable form of this nutrient.
Most tea is fermented. Fermentation intensifies the stimulant properties of the leaves and produces black and oolong varieties. Green teas are the unfermented leaves of Camellia sinesnsis.
As with all products containing living bacteria,probiotic products must be cooled during storage. If heated, they won’t survive. This includes pasteurization.
Prebiotics
Prebiotics help keep probiotics alive. We don’t digest prebiotics, which come mainly from oligosaccharides (complex starches), but probiotics love them.
Inulin and fructo-oligosaccharides (FOS) are common prebiotics. You’ll get them from legumes, fruits and whole grains. They are abundant in the food supply (assuming you eat real food). Oh, another prebiotic is galacto-oligosaccharide (GOS), found in human breast milk. Hooray for breastfeeding.
| Prebiotics | Probiotics | |
|---|---|---|
| What are they? |
|
Certain species/strains of:
|
| Food sources |
|
Bacteria
Yeasts, molds, and fungi
|
| Potential benefits |
|
|
Summary and recommendations
Probiotics seem to improve overall health, metabolism, immunity, digestion, and body composition. They may even help alleviate inflammatory conditions.
Getting probiotics from food:
If you are healthy, aim for 1-2 servings of probiotic rich foods each day (use the food source list above). If you’re hoping to prevent or alleviate a medical problem, you may need to increase the dose.
Getting probiotics from supplements:
Supplemental doses are typically expressed in billions of live organisms. Between 3 and 5 billion would be a starting dose. This could be increased to 10 billion if you are hoping to alleviate a specific health concern. Take with food/drink and use a reputable brand.
Getting prebiotics from food:
- If you are healthy, aim for 2-3 servings of prebiotic rich foods each day (use the food source list above).
Getting prebiotics from supplements:
2-4 grams of FOS per day can help to feed healthy gut bacteria and keep things balanced. Supplementing pre- and probiotics at the same time might be a good idea.
Take note: You may actually feel worse before you feel better since bacteria release toxins.
Immune-compromised individuals can develop infections from probiotic microbes – be cautious if you are taking immunosuppressive drugs, if you have AIDS, if you are receiving radiation or chemotherapy, and/or if you are in the hospital.
Extra credit
Probiotics are not digestive enzymes. Digestive enzymes are like chemical grinders that chew up substances and break them down for us so we can absorb them. For example, we can’t absorb big chunks of protein, so our body uses proteases — protein-breaking enzymes — to break them down into smaller parts that we can digest.
Even dead probiotics appear to have beneficial effects.
It appears that using probiotics during pregnancy is safe.
Together, all of the microbes in your body weigh about 3 pounds – more than your kidneys.
Side effects of antibiotics include diarrhea, yeast infections and oral thrush.
Eat, move, and live… better.©
Yep, we know… the health and fitness world can sometimes be a confusing place. But it doesn’t have to be.
Let us help you make sense of it all with this free special report.
In it you’ll learn the best eating, exercise, and lifestyle strategies — unique and personal — for you.
Click here to download the special report, for free.
References
Click here to view the information sources referenced in this article.
Share