What is diabetes mellitus?
Diabetes mellitus (DM) is a group of metabolic diseases characterized by high blood sugar resulting from defects in insulin secretion, insulin action, or both. Nearly 90% of patients with DM have Type 2 diabetes.
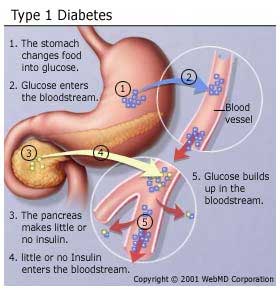
Type 1 DM is absolute insulin deficiency — in other words, the body cannot produce insulin. This is from a defect in the pancreas, the insulin-producing organ of the body. Type 1 DM is often understood to be an auto-immune disorder, in which the body destroys its own tissue (in this case, the cells of the pancreas).
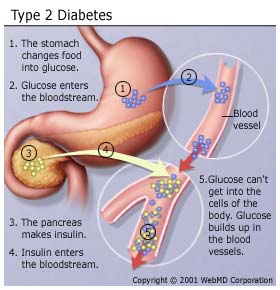
Type 2 DM arises because of insulin resistance. In this case, the body may be producing insulin but cannot use it properly. These individuals usually carry excess body fat; 80% of clients with Type 2 DM are obese at onset.
|
|
|
Why is diabetes mellitus so important?
Over 20 million people in the United States have DM. That is nearly 7% of the population. While risk of Type 2 DM goes up with age, younger people are increasingly susceptible because of poor dietary habits and inactivity. Ethnicity can also affect one’s risk: US survey data shows that Natives (in some regions), African Americans, and Hispanics have higher than average rates of DM. Indeed, among people with Native ancestry living in Southern Arizona, rates of DM average 29% — nearly one-third of the population! [1]
DM drastically increases the risk of premature death and disability. Overall, the risk for early death among people with DM is about twice that of people without DM of similar age. If someone has high uncontrolled blood sugar levels for an extended period of time, it can result in organ damage, dysfunction, and failure. DM is linked to many serious health conditions.
For example:
- At least 65% of people with DM die of some form of cardiovascular disease (heart attacks, strokes, etc.).
- DM is the leading cause of new cases of blindness among adults aged 20 to 74 years. Diabetic retinopathy causes 12,000 to 24,000 new cases of blindness each year.
- DM is the leading cause of kidney failure. 44% of cases of kidney failure are due to DM. High blood pressure, which also occurs with DM, contributes to this.
Other potential complications of DM include:
- Growth impairment
- Obesity
- Ketoacidosis
- Greater infant mortality (gestational DM)
- Non-functional intestines
- Nervous system disorders and neuropathies
- Poor circulation
- Amputations (as a result of poor circulation and neuropathy; extremities often become infected or gangrenous)
What you should know
Type 2 DM is rampant, but almost entirely preventable — indeed, the vast majority of Type 2 DM cases could be prevented by the adoption of a healthy lifestyle.
Nutritional modifications for DM should be tailored to clients’ treatment goals and outcomes. While many professionals will make statements such as “low carb” or “low fat” diets are best for everyone, these claims are unsubstantiated. However, as researchers writing in the Canadian Journal of Diabetes remark in a recent literature review, reducing carbohydrate intake overall does appear to be more effective than reducing fat intake.
Emerging evidence suggests that in the short term (within 6 months), when substituted for a conventional low-fat diet, low-carbohydrate diets can result in greater weight loss and better glycemic control, without a negative effect on blood lipids. There is, however, insufficient research to evaluate long-term risks or benefits. Individuals with type 2 diabetes who significantly restrict food groups or specific foods should have their diets assessed for fibre, antioxidant, nutrient and folate content.[2]
Another study in the British Journal of Nutrition points out that the type of carbohydrate is also relevant. Researchers found that diets high in refined sugars and starches (such as baked goods, sweetened drinks, etc.) had a different effect than diets where carbohydrates came from high-fiber, low-glycemic-index foods (e.g. foods such as vegetables, whole grains, etc.).
The detrimental effects of a high-carbohydrate diet on plasma glucose/insulin, triglyceride/HDL or fibrinolysis [the breakdown of blood clotting products] occur only when carbohydrate foods with a high glycaemic index are consumed, while they are abolished if the diet is based largely on fibre-rich, low-glycaemic-index foods. [3]
A recent PN Research Review looked at a study that compared the effects of a low-carb, low-fat, and Mediterranean diet on various blood measures and found that a combination of low-carb and Mediterreanean diets scored highest for the measures important to diabetics — blood sugar control, reduction in waist circumference, etc.
Thus, based on the existing evidence, it appears that people wishing to manage their insulin sensitivity and Type 2 diabetes must consider both amount and type of carbohydrate.
It also appears that simply losing weight will help restore (or at least significantly improve) normal glucose tolerance and blood sugar levels.
Most importantly, any method of DM management must accomplish the following goals:
- Maintain near normal blood sugar levels (80-120 mg/dl fasting), and less than 7% HbA1c
- Normal serum lipid levels
- Healthy blood pressure
- Reduce body weight and body fat levels to healthy range
Blood sugar levels and medication
It’s important to recognize the signs/symptoms of high and low blood sugar levels. This can allow for the proper treatment.
| Signs of high blood sugar | Signs of low blood sugar |
| Excessive hunger, excessive thirst, excessive urination, weight loss, weakness, infections, urinary ketones, blurred vision, cramps | Shaky, confused, hunger, weak, irritable, headache, tingling, nausea, double vision |
Insulin therapy may be initiated among individuals with Type 2 DM, and is all but certain in those with Type 1 DM. The insulin/diet correlation is vital. Too much insulin can cause extremely low blood sugar and death. Be sure to note insulin sources, speed of absorption, peak times of effect, and duration of effect.
Oral medications are generally used to control blood sugar levels in clients with Type 2 DM. Medications may slow sugar absorption, increase the tissues sensitivity to insulin, or alter the output of insulin from the pancreas. For more on oral medications, see here.
Exercise
Exercise is a cornerstone of DM care. It improves blood sugars, insulin sensitivity, reduces body fat, improves cardiovascular function, and reduces stress. The effect DM has on an exercise session depends on several factors including type of medication, timing of medication, blood sugar levels prior to exercise, previous food intake, and type of exercise.
General guidelines for regulating blood sugar response to exercise:
- Metabolic control before exercise
- Avoid exercise if fasting sugar levels are greater than 250 mg/dl and ketosis is present, and use caution if sugar levels are greater than 300 mg/dl and nketosis is present.
- Ingest added carbohydrate if sugar levels are less than 100 mg/dl
- Blood sugar monitoring before and after exercise
- Identify when changes in insulin or food intake are necessary
- Learn the blood sugar response to different exercise conditions
- Food intake
- Consume added carbohydrates, as needed, tavoid low blood sugar
- Have carbohydrate-based foods readily available during and after exercise
For extra credit
Ideas on how to prevent Type 1 DM:
- Encourage breastfeeding
- Avoid early introduction of cow’s milk
- Avoid early introduction of gluten-containing foods
All of these are linked to the prevention of early onset auto-immune conditions.
Vitamin C in high doses can give false-positive urinary glucose results.
Chromium may assist with blood sugar control.
Summary and recommendations
DM can be a devastating disease. Since about 90% of DM cases are Type 2, and since Type 2 is so easily prevented through lifestyle modifications, good nutrition and regular activity could drastically reduce the number of Type 2 DM cases. Practical strategies include:
- Maintain a healthy body fat level (or reduce your body fat level if necessary to a healthy range)
- Evenly space your meals
- Avoid alcohol
- Eat a fruit and or vegetable with every meal
- Eat a form of legumes every day
- Protein at most (if not all) meals
- Avoid trans fat consumption
- Exercise for at least 5 hours per week
- Avoid refined carbohydrates
- Consume no less than 25 grams of fibre per day
- Avoid processed foods
- Eat/supplement with foods containing omega-3 fats
The best news is that if you’re already living the PN lifestyle, you’re doing most of this. You’ve cut your risk dramatically, perhaps without even knowing it!
Eat, move, and live… better.©
Yep, we know… the health and fitness world can sometimes be a confusing place. But it doesn’t have to be.
Let us help you make sense of it all with this free special report.
In it you’ll learn the best eating, exercise, and lifestyle strategies — unique and personal — for you.
Click here to download the special report, for free.
References
Click here to view the information sources referenced in this article.
Share